Diplegic Cerebral Palsy (CP)
The diplegic type of CP is distinguished by the main anatomic distribution of involvement in the muscles of the trunk (usually low toned) and lower limbs (progressively high-toned). Though the incidence is declining, diplegia occurs in about 35% of the CP population. [1]
Applicable TheraTogs Systems
These TheraTogs products support therapy goals for children with diplegic CP:
- Posture and Torso Alignment (PTA) System
- Full Body System (FBS) (includes limb strapping components)
- Wunzi System (for infants and young preschoolers)
Management Contributions via TheraTogs
Competent limb use begins with trunk and pelvic alignment and postural control – the ability to sustain a posture while attending to and engaged in a purposeful activity.
These essentials are both learned and established using appropriate sensory input from the load-bearing and functioning muscles and joints, and when achieved, they deliver appropriate sensory input through the same receptors. Balance deficit, postural problems, and strength deficits are common issues in clients with diplegic CP.
We advocate enhancing the acquisition of trunk alignment and control by optimizing the functioning base of support if needed.
 Therefore, we recommend beginning to use TheraTogs garments to deliver abundant somatosensory input to the trunk and hips, with strapping applied to support the acquisition of the fundamental, core components of postural control – trunk extension and flexion – against gravity and in all positions.[1] (As shown at right.)
Therefore, we recommend beginning to use TheraTogs garments to deliver abundant somatosensory input to the trunk and hips, with strapping applied to support the acquisition of the fundamental, core components of postural control – trunk extension and flexion – against gravity and in all positions.[1] (As shown at right.)
Adjusting functioning limb alignment is secondary to torso alignment and corrected weight loading on the full surface of the feet, with an emphasis on loading the heels.
Example: In therapy sessions, begin to use strapping to align the hips while caretakers are learning to don the garments and torso strapping (bottom right)
Caution: If you plan to rotate the hips outward, do so gently for children of age >7 years to avoid stressing the hip joints.
Applicable Evidence, Science, and Therapy Approaches
Evidence. Read how an experienced pediatric PT trained in Neuro-Developmental Treatment used TheraTogs to supplement her therapy: Francesca Case Study.
Science. Learn more about how TheraTogs apply established scientific and therapeutic principles for children with diplegia:
- Biomechanics
- Kinesiology
- Postural control
- Somatosensory (information processing and modulation)
Therapy Approaches. These established therapy practices can be effective management approaches for children with diplegia:
- Movement System [Impairment Syndrome] Analysis and Management
- Neurodevelopmental Treatment (NDT)
- Perception-Action Approach (P-A) (formerly TAMO – Tscharnuter Akademie for Motor Organization)
More About Diplegic Cerebral Palsy
The main cause of diplegic CP is premature birth accompanied by a hemorrhage of blood vessels that leak into the ventricles in the brain and result in scar tissue formation (periventricular leukomalacia) in the nearby pyramidal (corticospinal, motor) tracts. [3]
Pyramidal tract lesions – however static and unchanging – are associated with an impaired ability to isolate the activation of muscles in a selected pattern in response to demands of a voluntary posture or movement (i.e. reduced selective motor control). Yet the lower limb muscle stiffness and joint deformities worsen over time.
The muscle and soft-tissue stiffness is commonly referred to as “spastic” – suggesting that stretch reflex hyperactivity is the cause – despite the well-documented progression of use-related stiffening that occurs in the muscles and neighboring connective tissues. If spasticity is present, it cannot cause deformity, and its influence on movement skill is minimal. The more important issues are the deficits in trunk control and in the use of the pyramidal tracts for selective motor control.[4],[5],[6]
Somatosensory and tactile processing deficits accompany this altered movement history. Muscle weakness is inevitable after a history of using compensatory strategies. [7]
The capacity of living tissues to adapt to a prolonged use history is well established. Children with diplegia, born prematurely, begin to use their muscles against gravity in different ways from those of their full-term peers whose lower limb muscles are tighter at birth after spending more time tucked into flexion in the uterus.
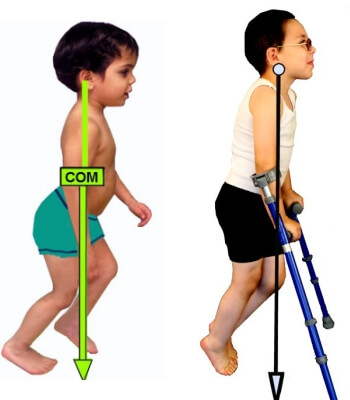 Early efforts to achieve the upright position in diplegic infants are compromised by a shortfall in the mechanical alignment factors of full-term gestation and of the fundamental components of trunk extension and flexion against gravity- the necessary ingredients for effective limb use.[8] Children with diplegia learn to use their limb muscles to varying degrees to maintain balance in sitting and standing positions. Limb muscles used chronically and tonically to stay upright become short and stiff over time. The muscles on the back side of the lower limbs work the hardest because children with diplegia carry their body weight in a forward lean.[9] (See image at right.)
Early efforts to achieve the upright position in diplegic infants are compromised by a shortfall in the mechanical alignment factors of full-term gestation and of the fundamental components of trunk extension and flexion against gravity- the necessary ingredients for effective limb use.[8] Children with diplegia learn to use their limb muscles to varying degrees to maintain balance in sitting and standing positions. Limb muscles used chronically and tonically to stay upright become short and stiff over time. The muscles on the back side of the lower limbs work the hardest because children with diplegia carry their body weight in a forward lean.[9] (See image at right.)
One might regard compromised postural control as the primary problem that promotes walking difficulty and stiff limb muscles due to a reliance on extensor muscles to remain upright, and due to the chronic use of limb muscles – rather than trunk muscles – to stay upright.
This brilliant insight regarding the persistent anterior displacement of the body center of mass in children with diplegic CP is the brainchild of the late Mary Weck, PT and the late Moira Tobin-Wickes, PT/CO of Children’s Memorial Hospital (now the Ann & Robert H. Lurie Children’s Hospital of Chicago).
The report by Sisson et al (1994)9 should inspire clinicians using gait analysis laboratories to determine the projection of the body COM onto the base of support in all children with movement disorders that feature increasingly stiff contractures in the muscles used to maintain the upright position.
Learn more about diplegic CP at CerebralPalsy.org and www.aacpdm.org.
References
- Odding E, Roebroeck ME, Stam HJ. 2006. The epidemiology of cerebral palsy: incidence, impairments and risk factors. Disabil Rehabil. 28(4): 183-91. Review.
- Pandyan AD, Gregoric M, et al. 2005. Spasticity: clinical perceptions, neurological realities and meaningful measurement. Disabil Rehabil. 27(1-2):2-6.
- Nardone A, Galante M, Lucas B, Schieppati M. 2001. Stance control is not affected by paresis and reflex hyperexcitability: the case of spastic patients. J Neurol Neurosurg Psychiatry.70(5): 635-643.
- Dietz V, Sinkjaer T. 2012. Spasticity. Handb Clin Neurol. 2012;109:197-211. Review.
- Damiano DL, Quinlivan J, Owen BF, Shaffrey M, Abel MF. 2001. Spasticity versus strength in cerebral palsy: relationships among involuntary resistance, voluntary torque, and motor function. Eur J Neurol. Nov;8 Suppl 5:40-9.
- Bly L. 2011. Components of Typical and Atypical Motor Development. Laguna Beach, CA; Neurodevelopmental Treatment Association; www.ndta.org
- Sisson G, Weck M, Prihoda W, Vankoski S, Kelp-Lenane C, Moore C, Weyers, 1994. The effect on gait of an anterior placement of the whole body center of mass. Gait Posture 2 (1): 56. [Poster]

